Radioisotopes for diagnostics
Nuclear medicine uses radioisotopes to diagnose diseases of the thyroid gland and other organs such as the lungs, heart, liver, gall bladder and skeletal system.
The most important and most frequently used isotope in nuclear medicine is technetium-99m, the daughter isotope of molybdenum-99 (Mo-99). It is used very widely for diagnostic purposes and is usually produced as a fission product during the irradiation of uranium. The radioisotope Tc-99m is used in up to 80% of applications of in-vivo diagnostics. This corresponds to more than 30 million tests worldwide each year.1 In Germany alone, about 60,000 tests a week are performed using Tc-99m.2 This corresponds to about one-tenth of the world's demand for Tc-99m. It is used mainly for the investigation of thyroid function, but also for the diagnosis of diseases of other organs such as the lungs, heart, liver, gall bladder and the skeleton.
In the future, molybdenum-99 will also be produced in large quantities at the FRM II.
Mo-99 production by irradiation
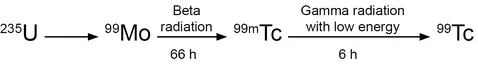
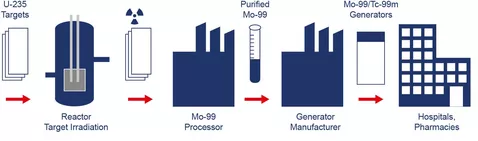
The most efficient and widely used method for the production of Mo-99 / Tc-99m is nuclear fission. The manufacture of Tc-99m involves the fission of U-235 to the fission product Mo-99, which decays to Tc-99m with a half-life of 66 hours. Tc-99m itself decays with a half-life of 6 hours to Tc-99 while emitting low energy gamma radiation. The half-life is the time in which half of the radioactive material decays. Since both Mo-99 with 66 hours and Tc-99m with 6 hours have short half-lives, it is immediately clear that the most widely used radioisotope in medicine, Tc-99m, cannot be stored. Therefore, the various steps in the production chain must proceed swiftly and be well-coordinated in order to supply hospitals with the necessary amount of Tc-99m at the right time.
After irradiation of the U-235 targets (Al-coated plates or tubes), they are subsequently chemically dissolved in a specially equipped device (processor) where the Mo-99 bound in the target is separated. For use in hospitals, the Mo-99 comes in so-called Mo-99 / Tc-99m generators where the Mo-99 decays to Tc-99m, which is then eluted or "milked" on-site at the hospital. Depending on the application, the Tc-99m can then be attached to a suitable "smart" carrier molecule, which later recognizes, for example, tumour cells in a patient and docks with them. The patient is injected with Tc-99m with or without a pharmaceutical label. In decaying toTc-99,Tc-99m emits γ-radiation, which is then measured depending on the location. The short lifetime of 6 hours of the diagnostic or therapeutic isotope Tc-99m and the low energy of the γ-rays minimize the exposure of the patient to radiation.
Significant contribution of the FRM II to security of supply Mo-99 / Tc-99m
Due to the transient nature of the initial isotope Mo-99 and the high demand for Mo-99 / Tc-99m, Europe – and also Germany as the largest single consumer – requires its own medium and long term secured supply chain for Mo-99 / Tc-99m. With the completion of the Mo-99 irradiation facility currently under construction, the FRM II will significantly contribute to the supply security of Mo-99 / Tc-99m in Germany and Europe.
Global efforts to ensure the supply of Mo-99 / Tc-99m
Worldwide, the current and future operators of irradiation facilities for the production of Mo-99, as well as representatives of all partners in industry involved in the production chain, are working together in a group set up by the OECD / NEA, the so-called HLG-MR (High-level Group on the Security of Supply of Medical Radioisotopes), to ensure the sustainable delivery of the radioisotope Mo-99 / Tc-99m in future years. The results of this group are regularly published by the OECD / NEA on their websites.